
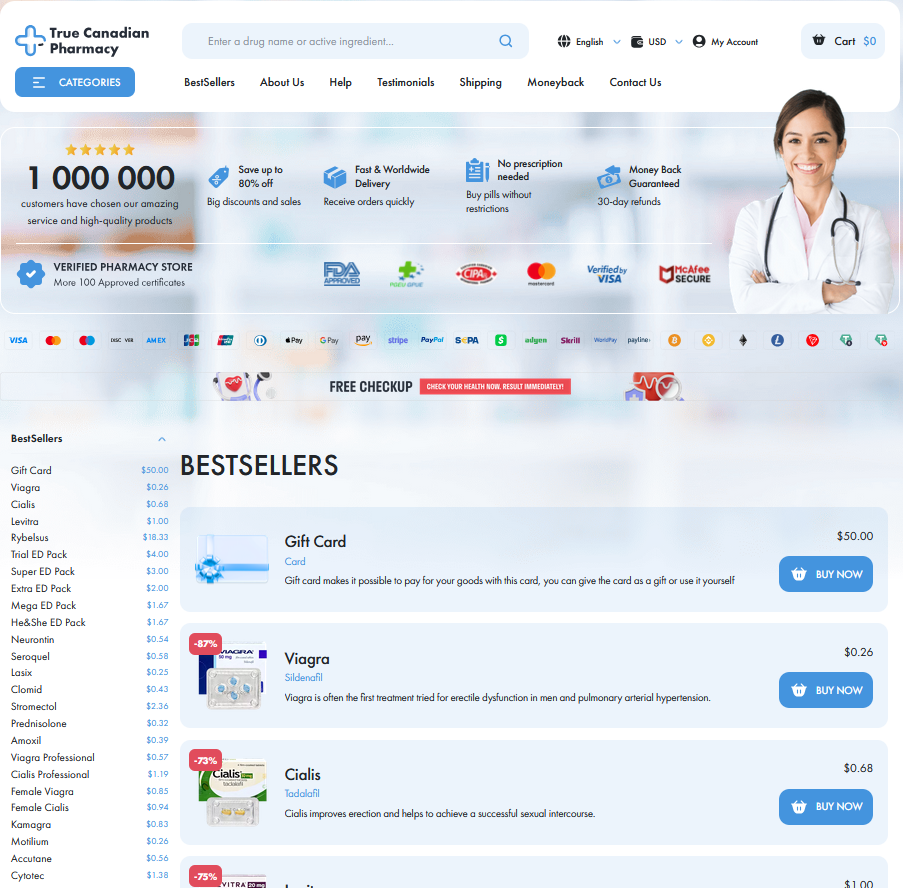
To Buy Priligy Online Visit Our Pharmacy ↓
 Priligy for Premature Ejaculation: Evidence Summary
Priligy for Premature Ejaculation: Evidence Summary
How Priligy Works: Mechanism and Pharmacology
Teh compound is a short-acting selective serotonin reuptake inhibitor (SSRI) developed for on-demand dosing. It is rapidly absorbed with peak plasma concentrations in about one to two hours and a terminal half-life of roughly 1.5 hours, supporting single‑dose administration.
Mechanistically it increases synaptic serotonin by blocking the serotonin transporter, enhancing activation of 5-HT1A and 5-HT2C receptor pathways that inhibit the spinal and brainstem ejaculatory circuitry. This modulation reduces seminal emission and delays the ejaculatory reflex.
Pharmacokinetically it is metabolized primarily by CYP3A4 and CYP2D6, with limited accumulation due to rapid clearance. Clinicians should consider interactions with strong CYP inhibitors and adjust expectations for time-to-effect; cardiac and drug interaction profiles guide selection and counseling on timing.
Clinical Trial Results: Efficacy and Time Gains

Early trials showed priligy increased intravaginal ejaculatory latency time for many men, transforming brief encounters into more satisfying sessions. Participants reported measurable gains and renewed confidence in sexual routines.
Randomized studies compared single-dose and daily regimens, noting variable effect sizes but consistent time gains. Benefits were dose-related and seen across age groups, though response varied individually.
Teh safety signals were mild: nausea, dizziness, and headache were common and occassionally led to discontinuation. Long-term surveillance suggests no major harms, but continued monitoring remains important for clinicians in routine clinical practice globally.
Safety Profile: Side Effects and Long-term Risks
A patient narrative often begins with hope: priligy can meaningfully delay climax, yet users describe dizziness, nausea, and sleepiness. Those early impressions shape expectations and shared stories in clinics.
Less common reactions include palpitations or sexual dysfunction persisting after treatment, though serious events are rare. Monitoring and clear counselling reduce anxiety and help identify adverse trends early.
Long-term data are limited; doctors weigh benefits against risks for each patient, considering comorbidities and concomitant medications. Occassionally dose adjustments or stopping the drug are the preferred Managment strategy. Regular follow up helps.
Comparisons: Priligy Versus Other Treatment Options

A patient’s choice often reads like a short story: priligy delivers rapid, on-demand control while daily SSRIs offer steady state improvements with delayed onset. Topical anesthetics numb local sensation but can reduce pleasure, and behavioral techniques teach control without drugs. Efficacy, speed, and partner factors shape decisions.
Clinicians weigh side effects, interactions, and patient preference; priligy is attractive for quick effect, but occassionally causes dizziness or nausea. Cost, comorbidities, and aparent expectations matter. Shared decision making and monitoring optimise benefits while minimising harms and follow-up improves long-term outcomes.
Dosage Strategies: Timing, Titration, and Patient Factors
In practice, dosing is a matter of personal tuning: most men start with 30 mg of priligy taken 1–3 hours before intercourse; if response is suboptimal after several uses and tolerated, clinicians may increase to 60 mg. Do not take more than one dose per 24 hours and avoid combining with SSRIs, MAOIs, or strong CYP3A4 inhibitors.
Teh practical side includes tailoring for age, comorbidities and concomitant drugs: reduce caution in hepatic impairment, avoid in significant cardiac disease, and counsel about syncope, dizziness and nausea which may Occassionally limit use. Reinforce that efficacy often becomes evident after a few administrations, encourage trialing both doses under supervision, and carefully document any adverse events or drug interactions.
Practical Guidance: Prescribing, Counseling, and Monitoring
Start with a focused medical assessment: sexual history, comorbidities, current medications, and contraindications such as cardiac arrhythmias, severe hepatic impairment, and concomitant MAOI use. For most patients begin with thirty milligrams taken one to three hours before intercourse; increase to sixty milligrams if response is inadequate and tolerability is acceptable. Avoid chronic daily use and check for interactions with SSRIs, strong CYP3A4 inhibitors, and thioridazine.
Counseling frames success: set realistic expectations about modest IELT gains, discuss common side effects (nausea, dizziness, headache) and the small risk of syncope. Advise patients to avoid excess alcohol and to report prolonged dizziness or mood changes. Encourage partner involvement and combine with behavioral techniques if needed to boost outcomes; many men Recieve better results when medication is paired with therapy.
Arrange follow-up at four to twelve weeks; reassess benefit, harms and need. EMA - Priligy NCBI review on dapoxetine
